Posted on September 6, 2022

Posted 9/6/2022

By Alana Vega
ACNJ Health Policy Analyst and Youth Engagement Coordinator
Since the onset of the COVID-19 pandemic, the usage of healthcare delivered through video conferencing systems or telephone, also known as telemedicine or telehealth, has increased. Thanks to recent state legislation, New Jersey families -- including those on publicly funded health insurance such as Medicaid and CHIP -- may have telemedicine services reimbursed by private insurers and NJ FamilyCare. Previously, New Jersey permitted limited access to these sorts of services, particularly for those enrolled in Medicaid. For some, telemedicine may seem strange because of its unfamiliarity. Yet, practices across the country have long relied on telemedicine, particularly in rural areas.
Physical and Mental Health Services
Telemedicine services can be administered in a myriad of ways. For many, client/provider interactions over video conference systems like Zoom, Webex, and FaceTime likely come to mind. However, providers have reported success administering healthcare over traditional audio-only telephone calls. This practice is especially important when connecting with rural populations, older Americans and those without a reliable internet connection.
Internet Access and Telehealth Care
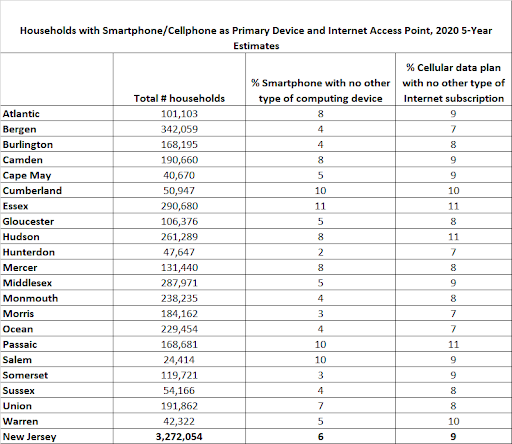
Although telehealth may be a means of increasing access to healthcare across the Garden State, concerns regarding internet and device access remain persistent. The “digital divide” is a term used to refer to the gap between those with internet and computer access and those without. In New Jersey, and across the country, data show that many households do have some type of internet access. According to the Pew Research Center, 93% of U.S. adults reported using the internet in 2021, compared to 76% in 2010. Data from the same set indicate that 15% of adults are smartphone-dependent--meaning they rely on their smartphones as their primary source of internet connection and do not have broadband internet at home.
Pre-pandemic, the majority of telemedicine visits were for urgent care needs; however, primary care visits, management of chronic conditions and specialist visits all saw an increase in telemedicine utilization post-2020. Physicians reported satisfaction with telemedical services--with more than 70% indicating a willingness to use technology for visits encompassing prescription renewals, chronic care management and/or post-surgical check-ins.
It is important to note that telehealth is not meant to replace in-person services entirely, but rather bolster the existing number of options offered to families. Some studies indicate patients were less satisfied with telehealth services. While not specific to children, one study demonstrated concerns among older, chronically-ill patients of color, who expressed difficulty building trust with their physician through a virtual visit. Another study points to a higher rate of antibiotic prescriptions than in-person care among children who attended virtual visits for respiratory infections. Unnecessary prescription of antibiotics has been cited by the Centers for Disease Control (CDC) as a factor contributing to antibiotic resistance, which could have a significant impact on the medical community’s ability to fight infections. There is also evidence showing that telehealth visits generate new concerns such as finding a quiet, solitary space for teletherapy visits to address mental health, protecting patient’s health information shared through telemedicine visits, and addressing gaps in familiarity with technology among patients and providers.
Despite some of the challenges associated with telemedical services, those specifically addressing mental health appear to have more widespread success--both from the patient and provider perspective. According to a Trilliant Health analysis of telehealth utilization between April 2019 and November 2021, behavioral health visits accounted for the single largest share of telehealth visits.
In their declaration of a national mental health emergency for children and teens, the American Academy of Pediatrics (AAP), the Children’s Hospital Association (CHA) and the American Academy of Child and Adolescent Psychiatry (AACAP) call for a variety of interventions and policy solutions to address the needs of young people. Among the list is a need to “address the regulatory challenges and improve access to technology to assure continued availability of telemedicine to provide mental health care to all populations.” A number of sources indicate that telemedicine can complement more traditional forms of mental health services or to provide specialized care for young people with specific needs.
In 2018, the New Jersey Pediatric Mental Health Care Access Program, managed by the New Jersey Chapter, American Academy of Pediatrics (NJAAP), utilized telepsychiatry to administer services to children in hubs across the state. Initially, a handful of the programs used video conferencing to see patients; as of April 2020, all nine hubs in the state leaned on telehealth services to reach their clients. Although some barriers were identified--limited office space for telepsychiatry visits as well as spotty or no internet access among patients--both providers and patients reported satisfaction with a number of features within the program. Telepsychiatry for children and adolescents, based on the experiences within the program, pointed to easier access to services through a reduction in transportation and scheduling barriers and more timely and appropriate referrals.
Among older youth ages 15-26, also known as “transition age youth”, telemental health is seen as an opportunity to bridge the gap in services offered to those transitioning from high school or college to career. Mental health services for this age group are in high demand, as many young people leave pediatric practices and begin to navigate the adult healthcare system on their own.
Conclusion
These findings for behavioral health services delivered through virtual systems come at a crucial time. In the final months of 2021, several authorities, including the CDC, AAP, CHA and AACAP, sounded the alarm for adolescent mental healthcare. The 2022 National KIDS COUNT Data Book points to a 40% increase in New Jersey children ages 3-17 with anxiety or depression, jumping from 7.6% of children in 2016 to 10.7%. More recent 2021 data, released by the Centers for Disease Control, show how the COVID-19 pandemic impacted high school students, with more than a third of those surveyed indicating poor mental health during the pandemic. As we enter a new school year--the second in-person instruction year since the pandemic began--assessing new methods of mental health service delivery to adolescents and young adults will be imperative.